Summary information and primary citation
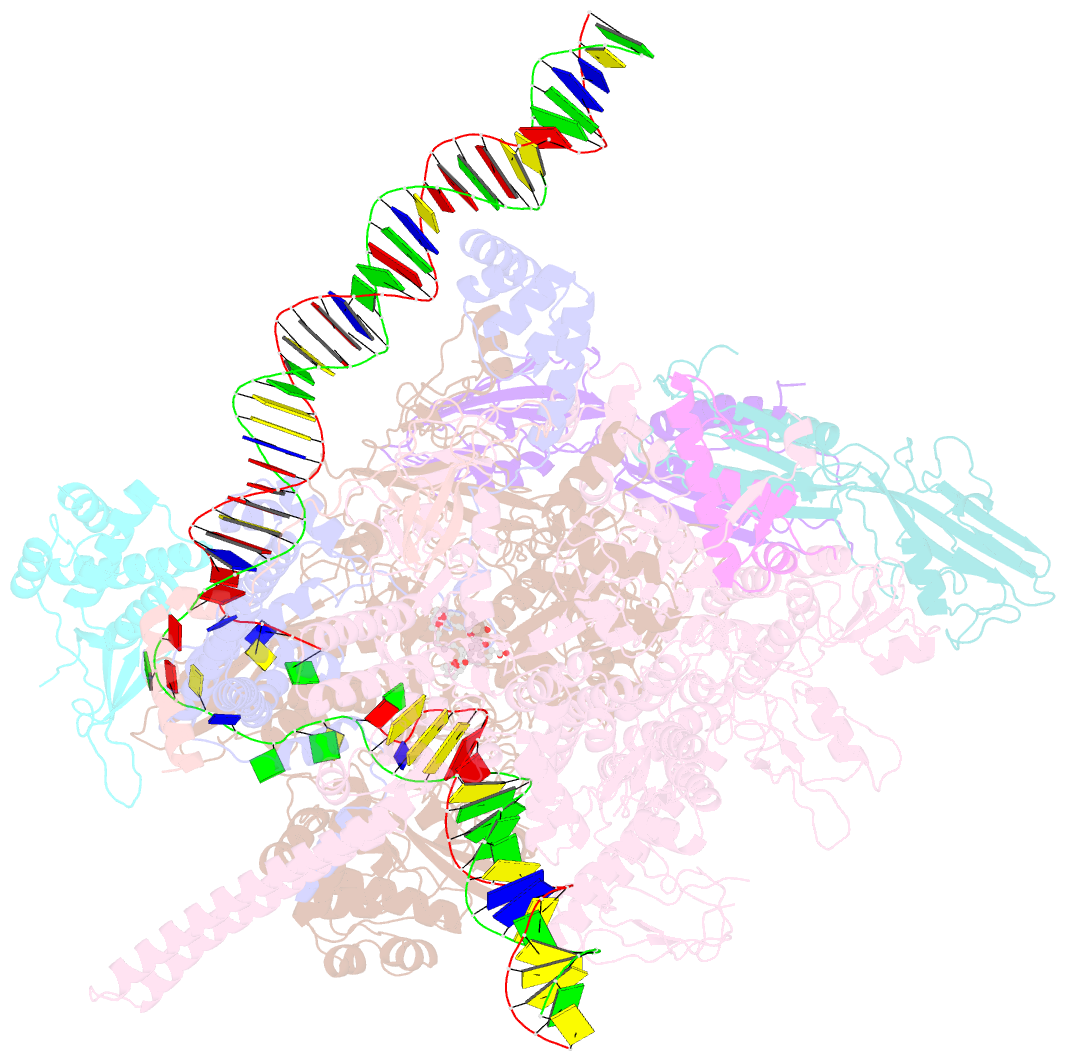
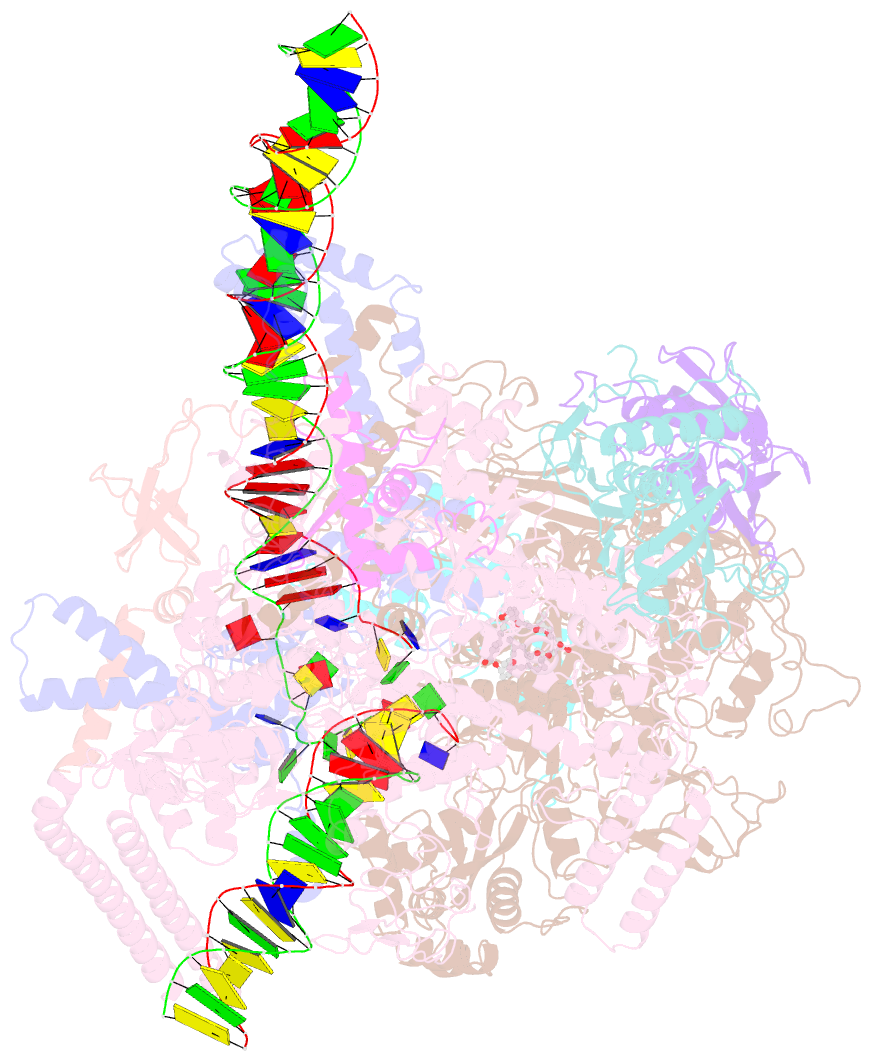
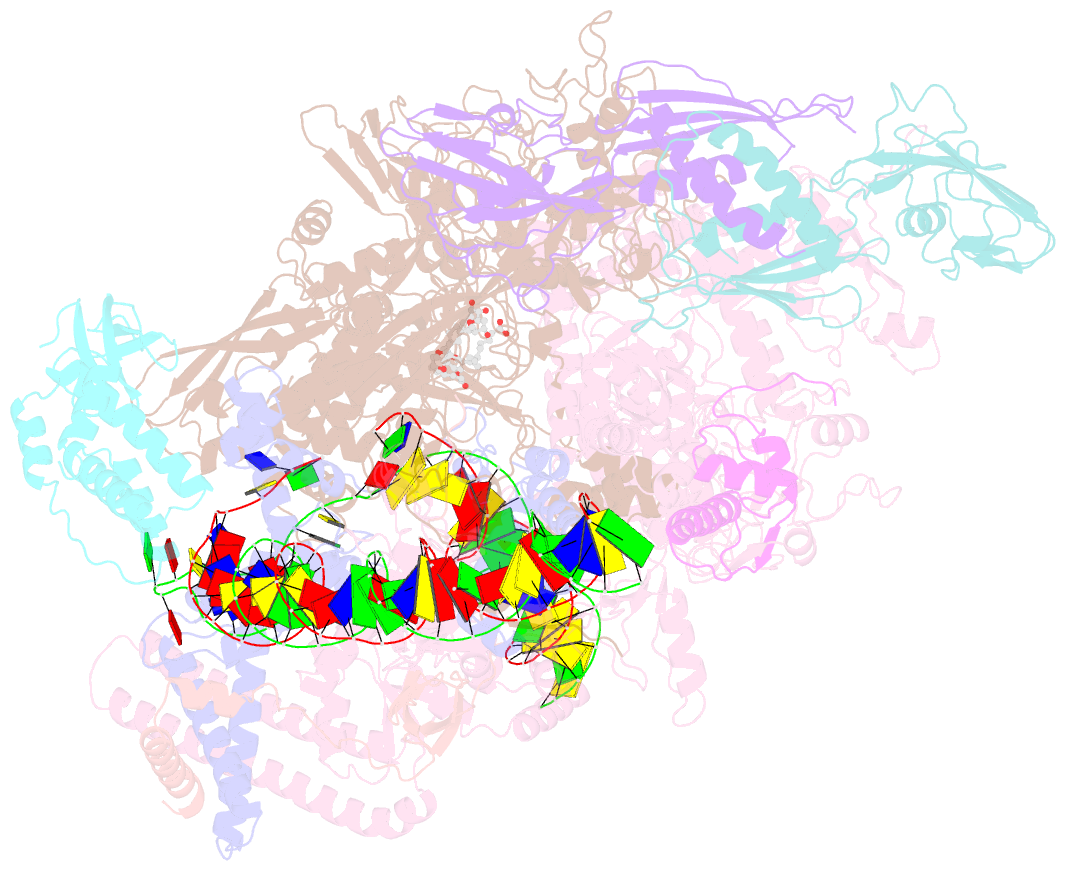
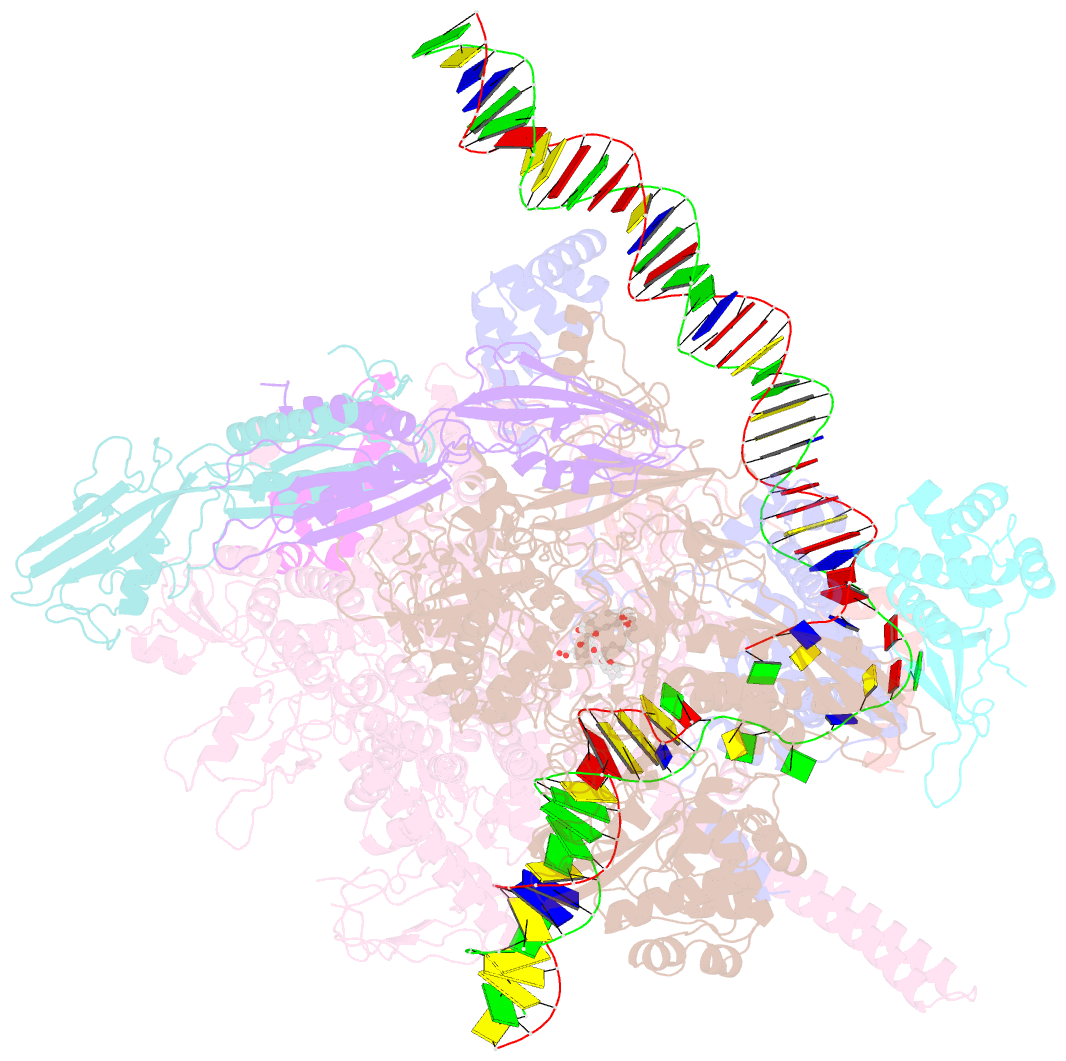
- PDB-id
- 6vvz; SNAP-derived features in text and JSON formats;
DNAproDB
- Class
- transcription,transferase-DNA-antibiotic
- Method
- cryo-EM (3.72 Å)
- Summary
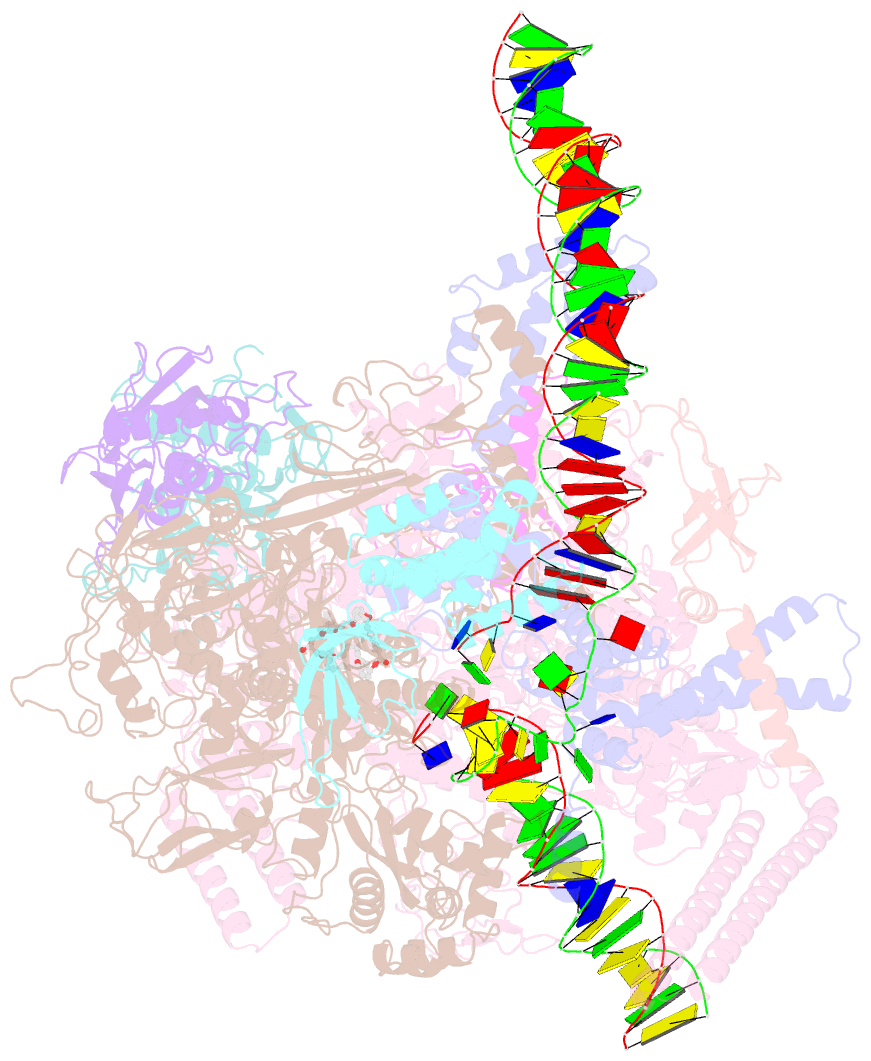
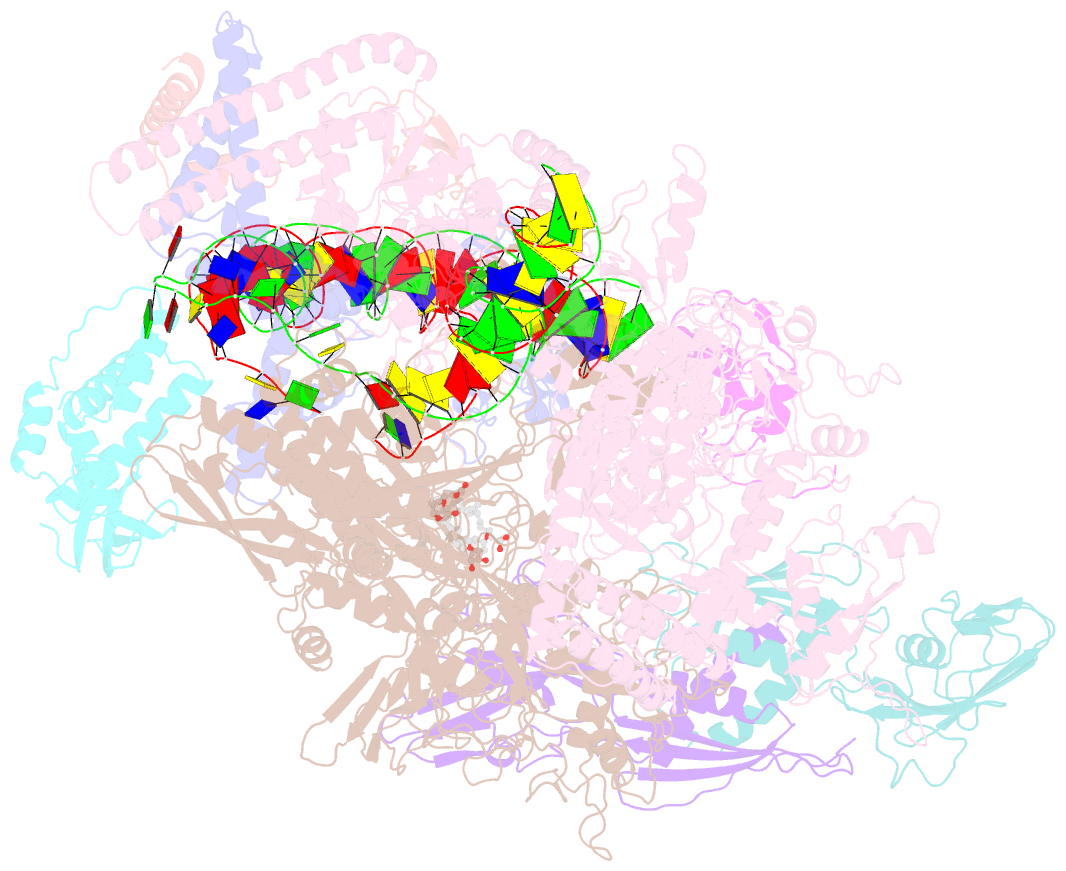
- Mycobacterium tuberculosis rnap s456l mutant transcription initiation intermediate structure with sorangicin
- Reference
- Lilic M, Chen J, Boyaci H, Braffman N, Hubin EA, Herrmann J, Muller R, Mooney R, Landick R, Darst SA, Campbell EA (2020): "The antibiotic sorangicin A inhibits promoter DNA unwinding in a Mycobacterium tuberculosis rifampicin-resistant RNA polymerase." Proc.Natl.Acad.Sci.USA, 117, 30423-30432. doi: 10.1073/pnas.2013706117.
- Abstract
- Rifampicin (Rif) is a first-line therapeutic used to treat the infectious disease tuberculosis (TB), which is caused by the pathogen Mycobacterium tuberculosis (Mtb). The emergence of Rif-resistant (RifR) Mtb presents a need for new antibiotics. Rif targets the enzyme RNA polymerase (RNAP). Sorangicin A (Sor) is an unrelated inhibitor that binds in the Rif-binding pocket of RNAP. Sor inhibits a subset of RifR RNAPs, including the most prevalent clinical RifR RNAP substitution found in Mtb infected patients (S456>L of the β subunit). Here, we present structural and biochemical data demonstrating that Sor inhibits the wild-type Mtb RNAP by a similar mechanism as Rif: by preventing the translocation of very short RNAs. By contrast, Sor inhibits the RifR S456L enzyme at an earlier step, preventing the transition of a partially unwound promoter DNA intermediate to the fully opened DNA and blocking the template-strand DNA from reaching the active site in the RNAP catalytic center. By defining template-strand blocking as a mechanism for inhibition, we provide a mechanistic drug target in RNAP. Our finding that Sor inhibits the wild-type and mutant RNAPs through different mechanisms prompts future considerations for designing antibiotics against resistant targets. Also, we show that Sor has a better pharmacokinetic profile than Rif, making it a suitable starting molecule to design drugs to be used for the treatment of TB patients with comorbidities who require multiple medications.